|
Button Battery Ingestion
Initial management
Imaging
Risk assessment
Management
Complications.
Esophageal Injury:
Post-Procedural Management:
Conclusion,
0 Comments
Guide for Patient Positioning
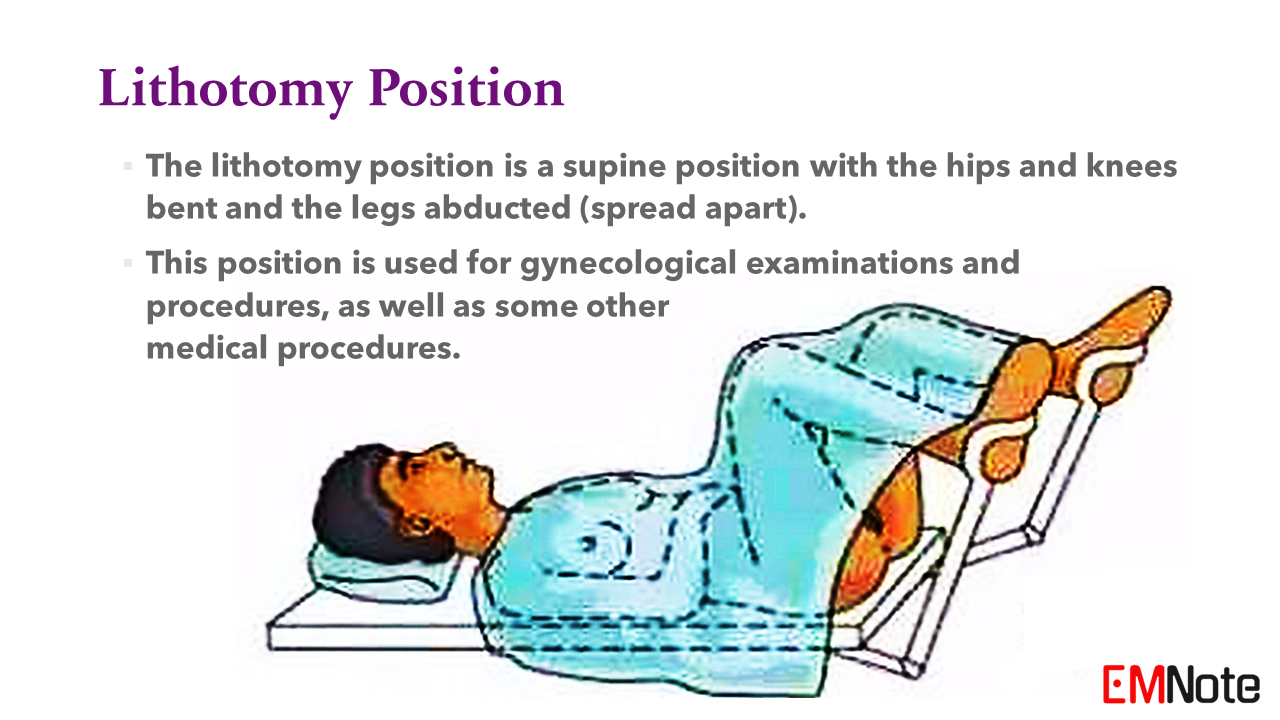
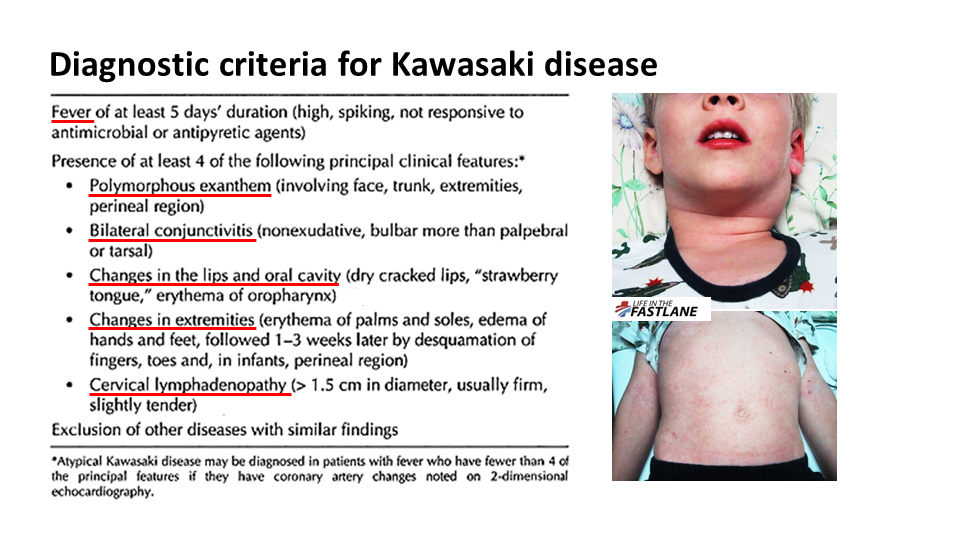
Supine Position * The supine position is when a person lies on their back with their face looking up. * This is the most common position for medical examinations and procedures. Prone Position * The prone position is when a person lies on their stomach. * This position is sometimes used for medical procedures, such as surgery on the back. Lateral Position * The lateral position is when a person lies on their side. * It is commonly used for sleeping but can also be used for medical procedures. * The left lateral position is preferred for pregnant women because it improves blood flow to the uterus and baby. Semi-Fowler position * The semi-Fowler position is a supine position where a person lies on their back with the head of the bed elevated between 30 & 45 degrees. * This position is often used to help people with breathing problems, such as heart failure or pneumonia. * It can also be used to improve comfort after surgery or during a long period of bed rest. Trendelenburg Position * The Trendelenburg position is a supine position with the head of the bed lowered and the foot of the bed elevated. * This position is used to improve blood flow to the head during surgery or shock. Reverse Trendelenburg Position * The reverse Trendelenburg position is a supine position with the head of the bed elevated and the foot of the bed lowered. * This position is sometimes used to improve blood flow to the legs during surgery. * It is also used for neck and head surgery and gynecological procedures because it reduces the flow of blood to those areas. Lithotomy position * The lithotomy position is a supine position with the hips and knees bent and the legs abducted (spread apart). * This position is used for gynecological examinations and procedures, as well as some other medical procedures. Jackknife position * The jackknife position is like a kneeling pose done lying down. * The patient lies on their stomach with hips bent high, and the head and legs are lowered. * This position allows surgeons better access to the abdomen and pelvis during certain procedures. Orthopneic position * The orthopneic position is a position that people with shortness of breath often assume to make breathing easier. * In this position, the person sits up with their feet supported on pillows or another surface. * This helps to open up the airways and improve airflow. Kawasaki Disease
Pathophysiology
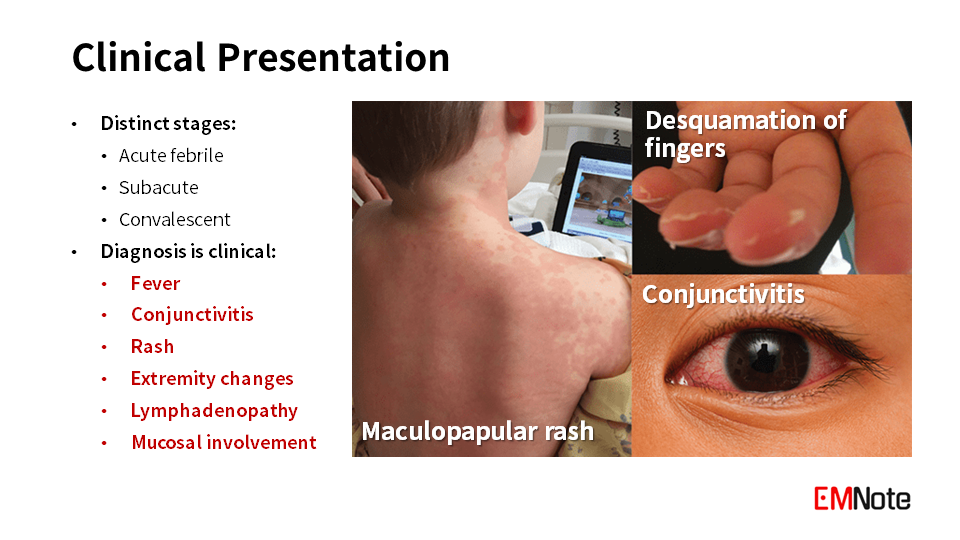
Clinical Presentation
Management
Prognosis
Take Home Message
E coli O157 H7 Infection
Clinical Presentation
Diagnosis
Treatment
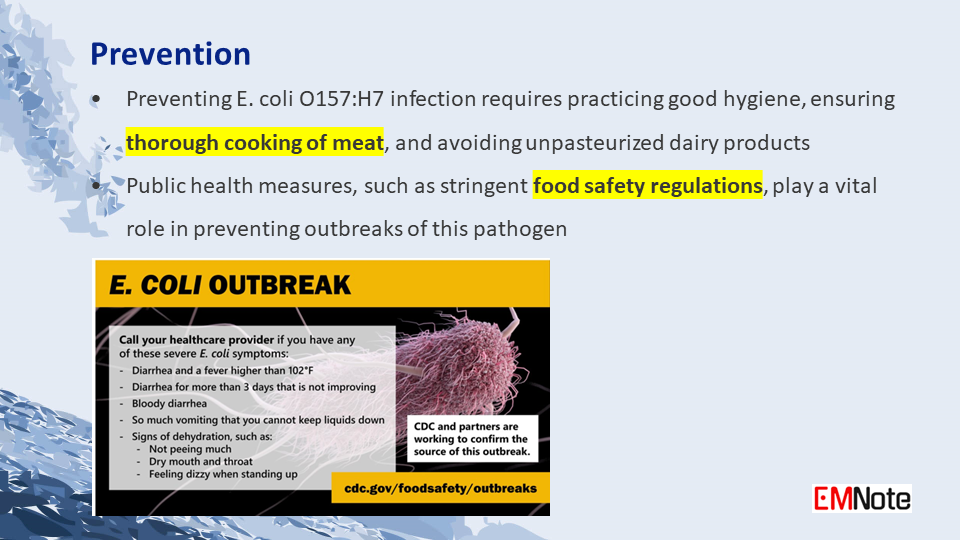
Prevention
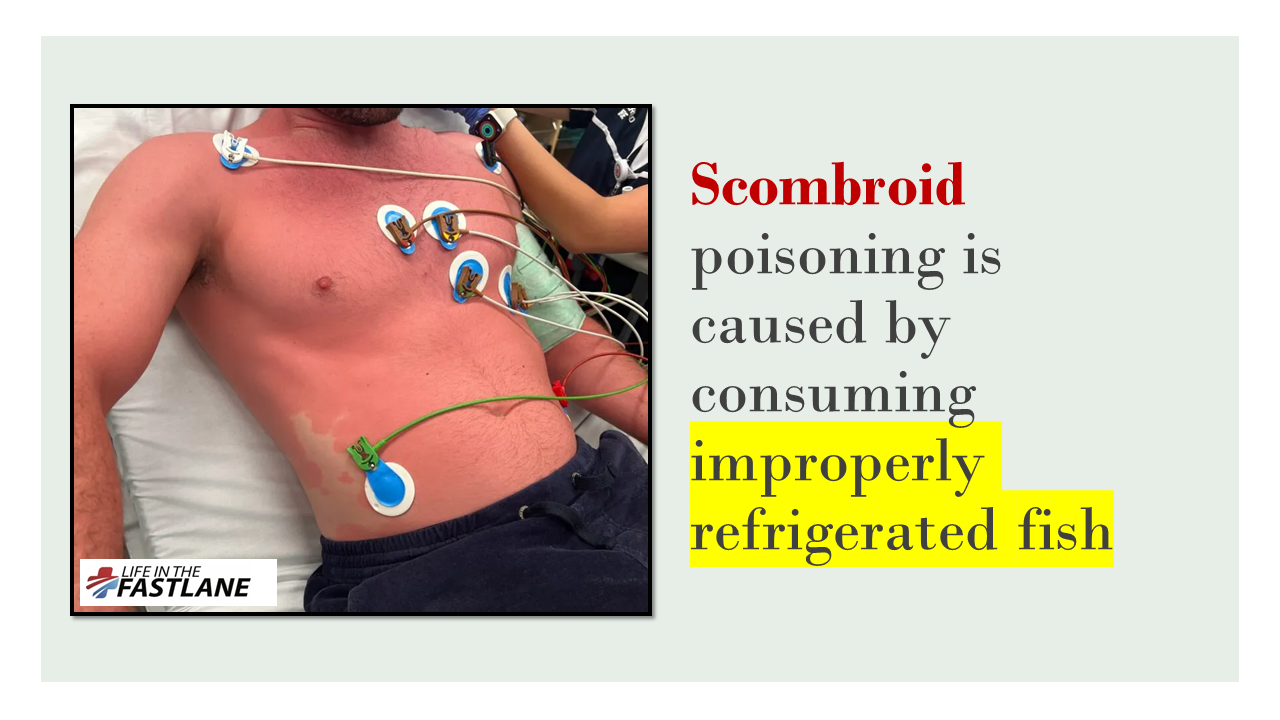
Scombroid and Ciguatera Fish Poisoning:
Scombroid Poisoning:
Ciguatera Poisoning:
|

Author
|
Proudly powered by Weebly