|
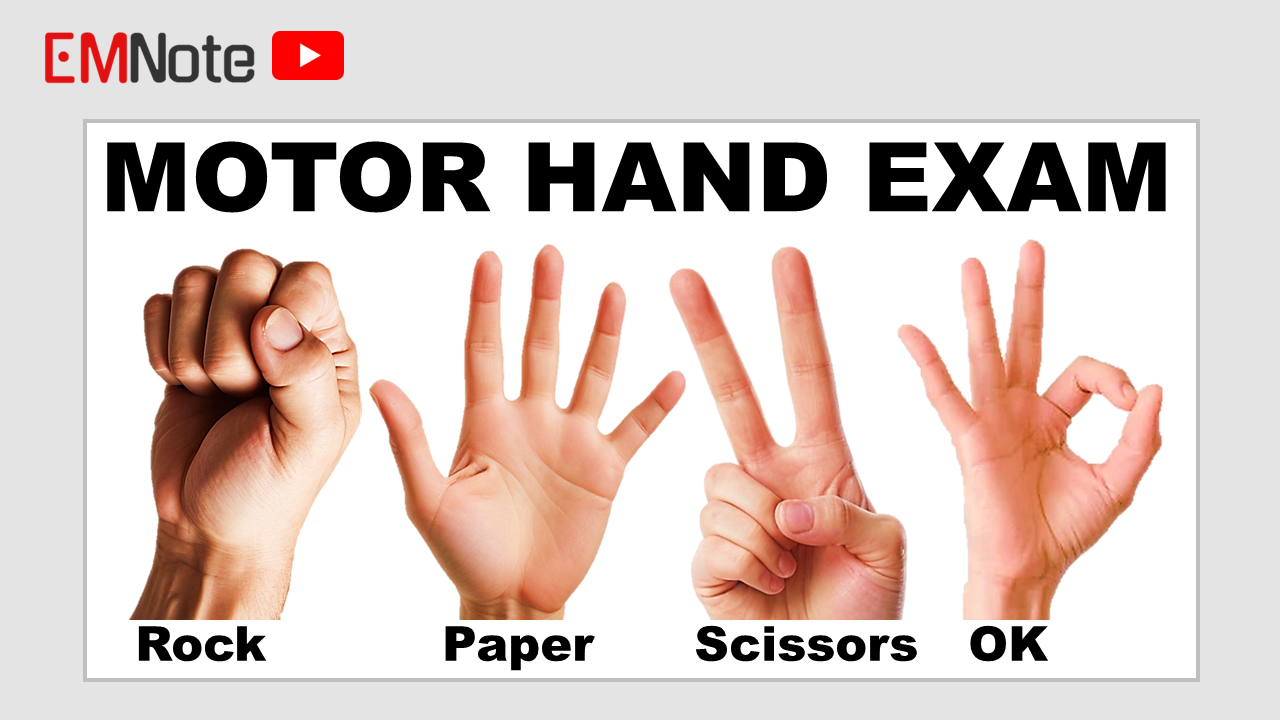
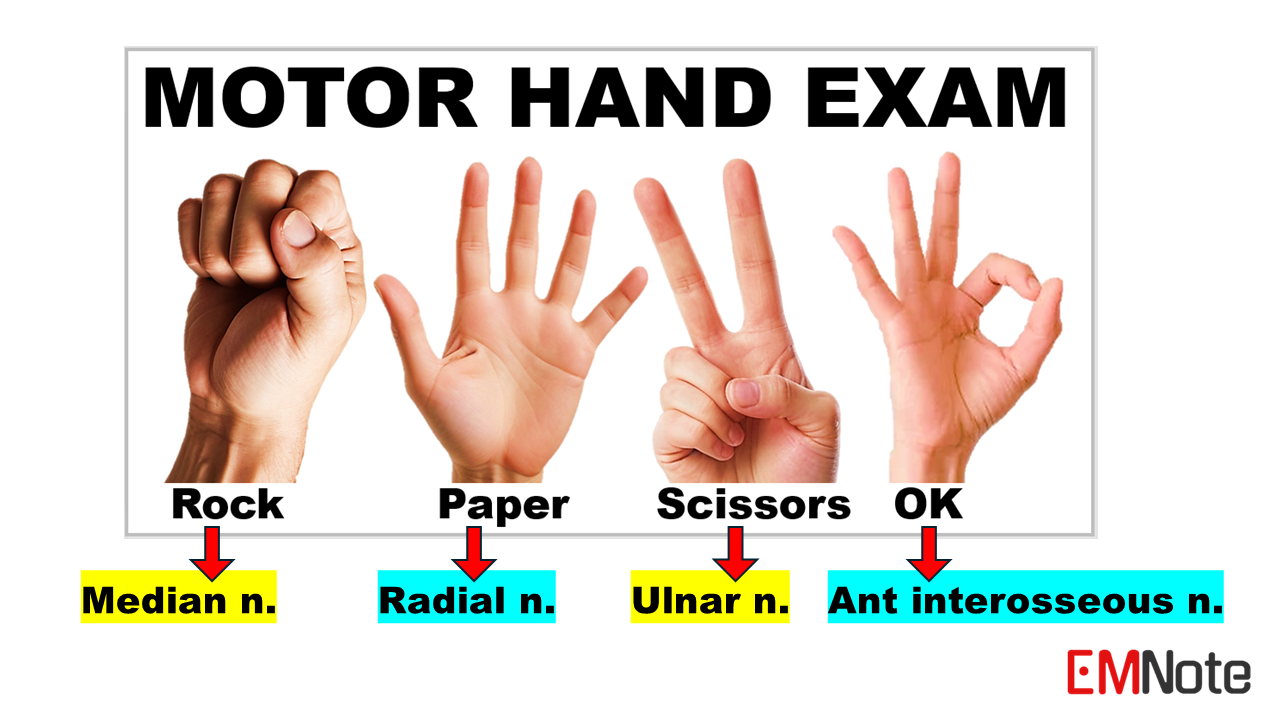
Motor Hand Exam
"Rock-Paper-Scissors-OK": A Mnemonic for Assessing Upper Limb Nerve Function
0 Comments
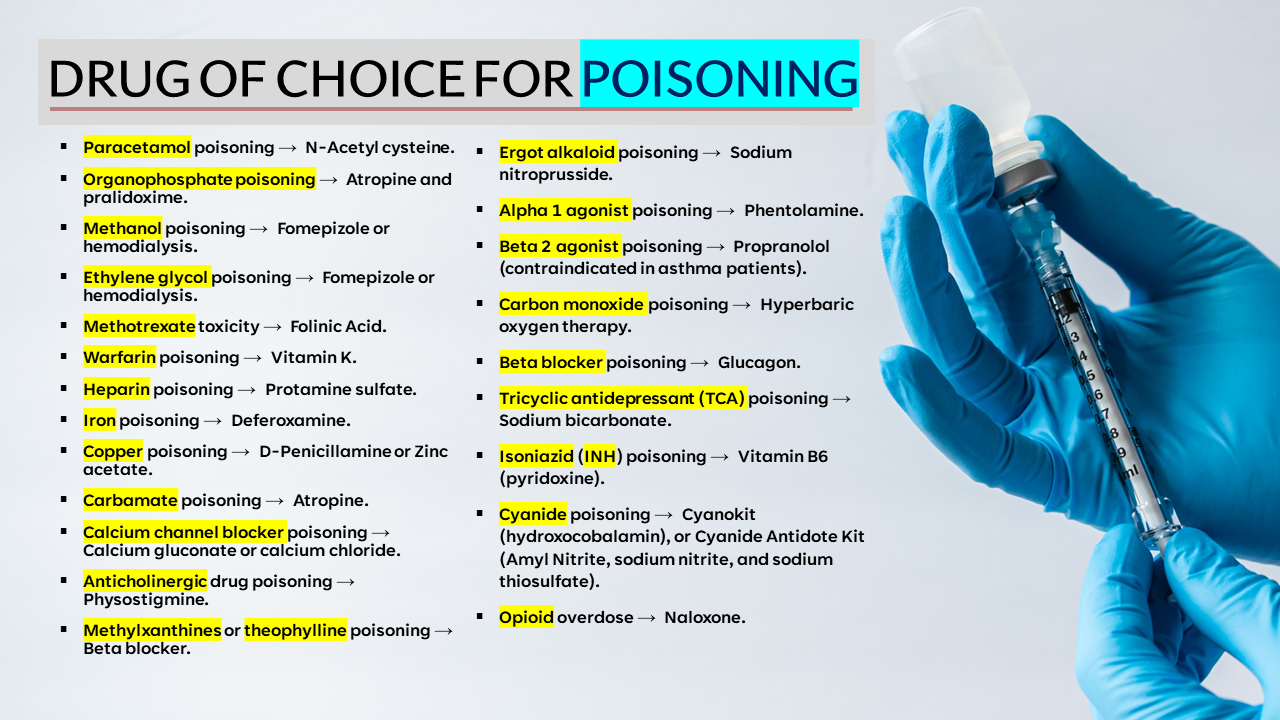
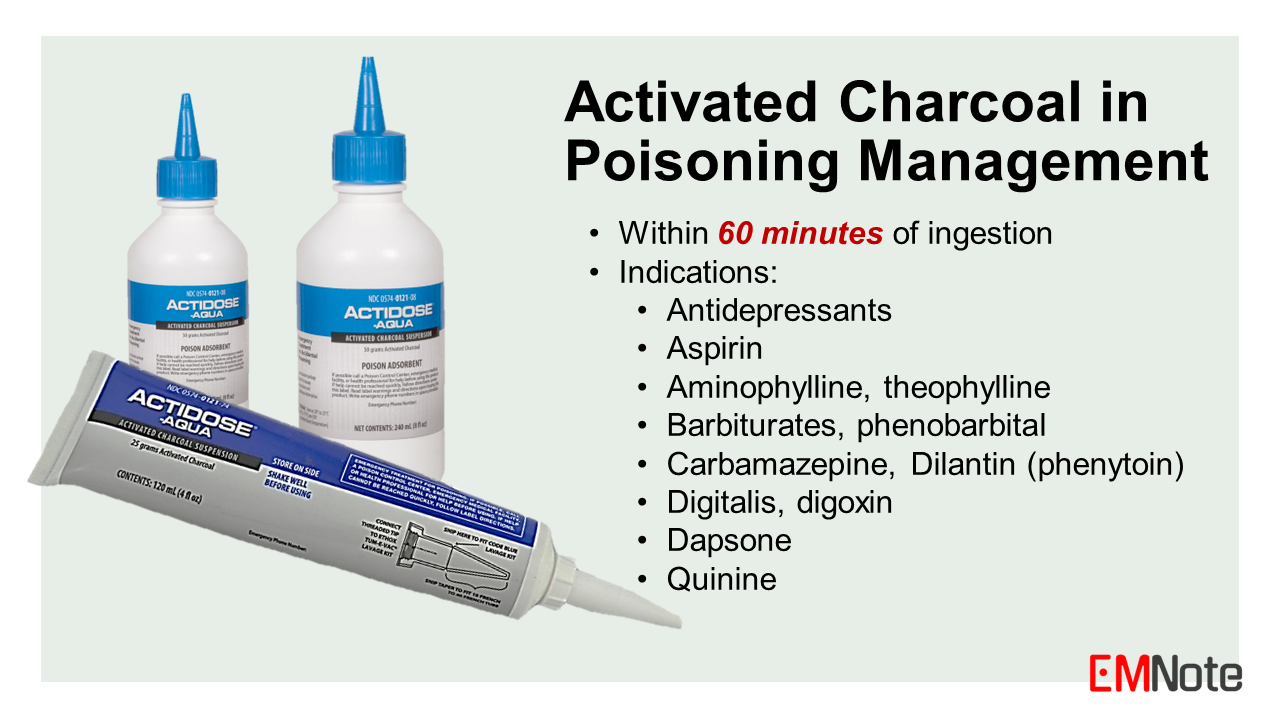
This is a list of DRUGS for POISONING TREATMENT:
"Educational Case Report" is dedicated to providing informative and engaging case reports across various medical disciplines. Our goal is to share real-world patient cases that offer valuable learning opportunities for medical students, healthcare professionals, and anyone interested in the field of medicine.
Chest X-Rays for Trauma
Activated Charcoal in Poisoning Management:
Dosage of Activated Charcoal The recommended dosage of activated charcoal varies depending on age:
Multidose Activated Charcoal
Complications of Activated Charcoal
Contraindications of Activated Charcoal
|

Author
|
Proudly powered by Weebly