|
Infective Endocarditis:
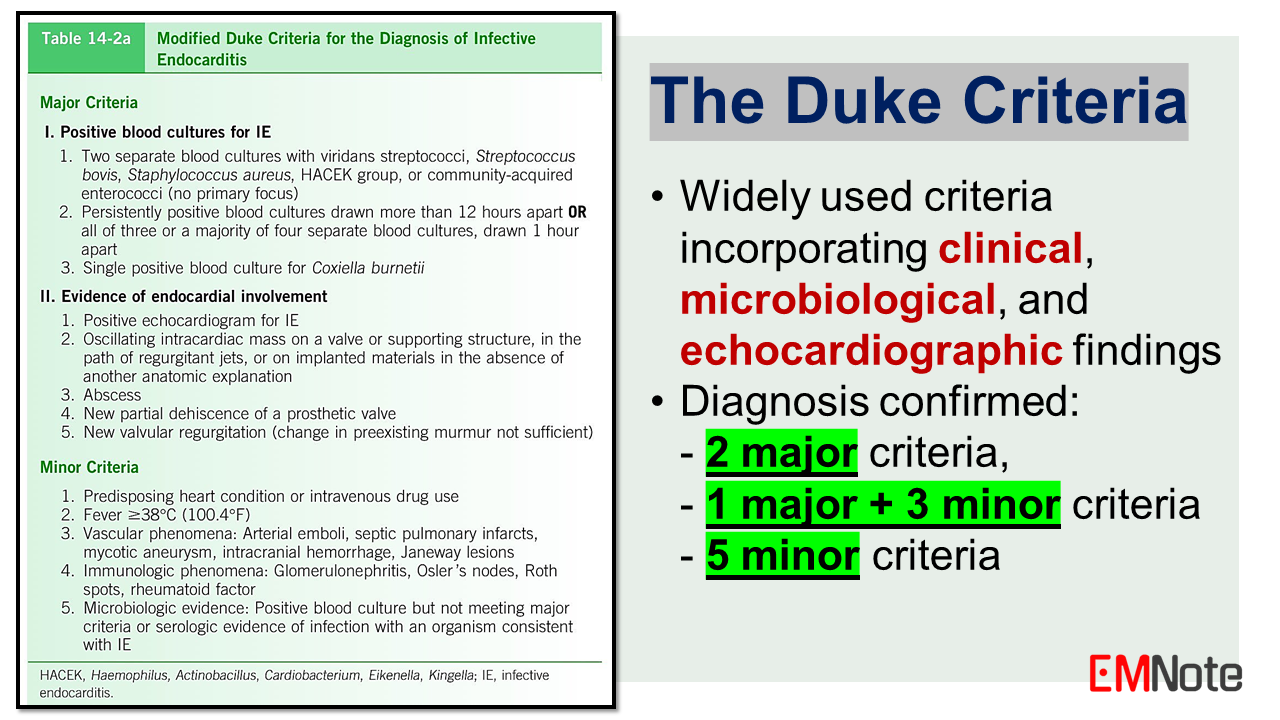
Epidemiology and Pathogenesis: IE predominantly affects individuals with predisposing cardiac abnormalities, such as congenital heart diseases, rheumatic heart diseases, prosthetic heart valves, or intracardiac devices. Intravenous drug abuse, indwelling catheters, poor dental hygiene, and immunocompromised states like HIV also increase the risk. The pathogenesis involves the formation of a platelet-fibrin vegetation on the endocardial surface, which serves as a nidus for bacterial colonization and proliferation, leading to tissue destruction and potential embolization. Causative Organisms: Staphylococcus aureus is the most common causative pathogen, accounting for approximately 30% of cases. Viridans group streptococci, enterococci, and coagulase-negative staphylococci are other frequently implicated microorganisms. The HACEK group (Haemophilus, Actinobacillus, Cardiobacterium, Eikenella, and Kingella) and fungi (Candida species) are less common etiologies. Clinical Manifestations: The clinical presentation of IE can be acute or subacute, depending on the virulence of the pathogen and the host's immune status. Common manifestations include fever, chills, malaise, anorexia, and weight loss. Cardiac manifestations may include new or changing murmurs, heart failure, or embolic events. Non-specific symptoms like arthralgia, myalgia, and back pain may also occur. The Duke Criteria: The Duke Criteria, established in 1994 and later modified in 2000, are widely used for the diagnosis of IE. These criteria incorporate clinical, microbiological, and echocardiographic findings. The diagnosis is confirmed by meeting two major criteria, one major and three minor criteria, or five minor criteria. Major Criteria include: 1. Positive blood cultures for IE pathogens. 2. Evidence of endocardial involvement on echocardiography, such as vegetations, abscess, or new valvular regurgitation. Minor Criteria include: 1. Predisposing cardiac conditions or intravenous drug abuse. 2. Fever. 3. Vascular phenomena, such as embolic events, Janeway lesions, etc. 4. Immunologic phenomena, such as glomerulonephritis, Osler nodes, Roth spots, etc. 5. Microbiological evidence not meeting major criteria. The Duke Criteria incorporate clinical, microbiological, and echocardiographic findings. The criteria demonstrate a sensitivity exceeding 90% for the diagnosis of IE. Management Principles: Early empiric antibiotic therapy is crucial, with vancomycin being the most appropriate choice for suspected IE due to its broad coverage of gram-positive organisms, including methicillin-resistant Staphylococcus aureus (MRSA). Subsequent antibiotic regimens should be tailored based on blood culture results and susceptibility patterns. Surgical intervention may be necessary in cases of refractory heart failure, uncontrolled infection, or high risk of embolization. Indications for surgery include valve dysfunction, perivalvular extension, or persistent bacteremia despite appropriate antimicrobial therapy. Prevention and Prophylaxis: Strict adherence to sterile techniques during invasive procedures and prompt management of bacteremia are crucial preventive measures. Antibiotic prophylaxis is recommended for individuals with specific high-risk cardiac conditions undergoing dental procedures or procedures involving manipulation of infected tissues.
0 Comments
Leave a Reply. |

Author
|
Proudly powered by Weebly