|
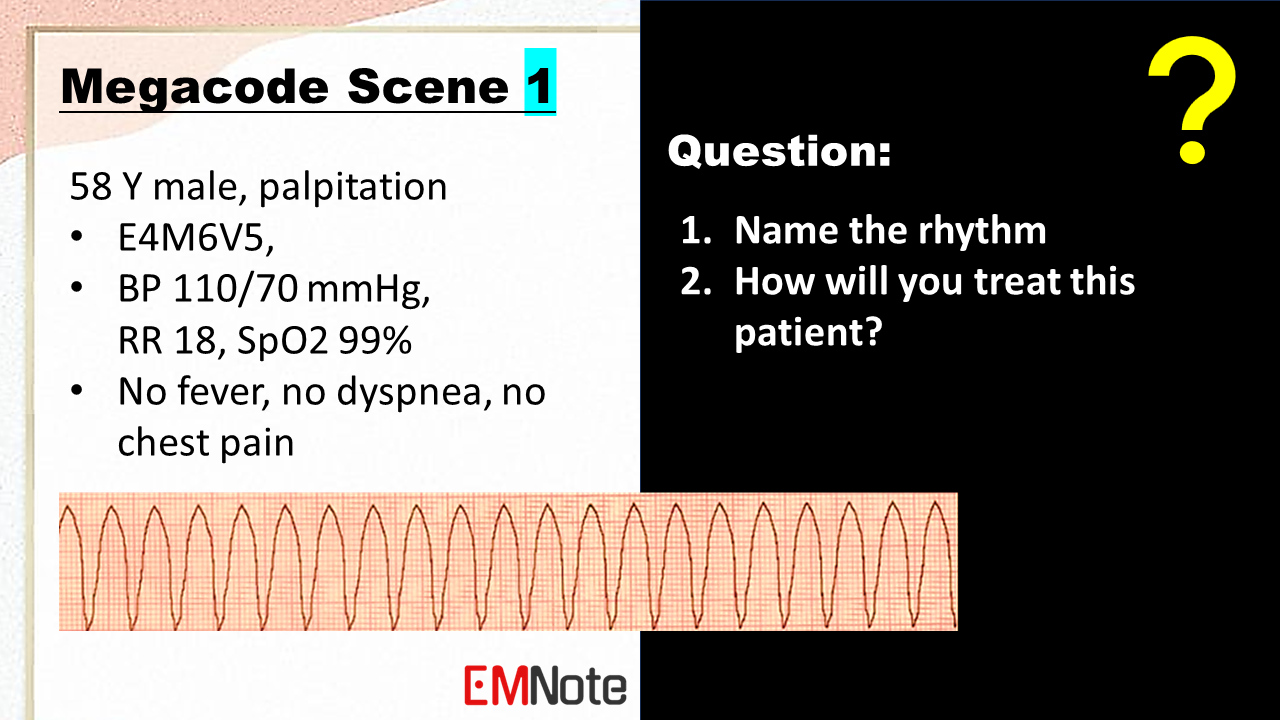
ACLS Megacode:
Initial Assessment: - Check for responsiveness, breathing, and pulse. - If unresponsive, call for help and initiate CPR. - Attach defibrillator pads and monitor. CPR: - Perform chest compressions at a rate of 100-120/min, allowing full chest recoil. - Provide rescue breaths at a ratio of 30:2. - Continue CPR until ROSC is achieved or until medical help arrives. Defibrillation: - If VF/VT is present, deliver a defibrillation shock of 360 joules biphasic or 360 joules monophasic. - If unsuccessful, increase the energy level to 400 joules biphasic or 400 joules monophasic and repeat. - Continue defibrillation attempts until ROSC is achieved or until medical help arrives. Emergency Medications: - Epinephrine: 1 mg IV/IO every 3-5 minutes. - Vasopressin: 40 units IV/IO every 3-5 minutes (if refractory to epinephrine). - Amiodarone: 300 mg IV/IO over 20 minutes (if refractory to defibrillation). - Lidocaine: 1 mg/kg IV/IO (if refractory to defibrillation). - Sodium bicarbonate: 1 mEq/kg IV/IO (if metabolic acidosis). - Calcium chloride: 10 mg/kg IV/IO (if hyperkalemia or calcium channel blocker overdose). Advanced Airway Management: - Intubate the patient if CPR is ineffective or if the patient is unable to maintain a patent airway. - Consider cricothyrotomy if intubation is unsuccessful. Post-ROSC Care: - Monitor vital signs closely. - Provide supportive care, including oxygen therapy, fluid resuscitation, and antibiotics. - Address any underlying medical conditions that may have contributed to the arrest.
0 Comments
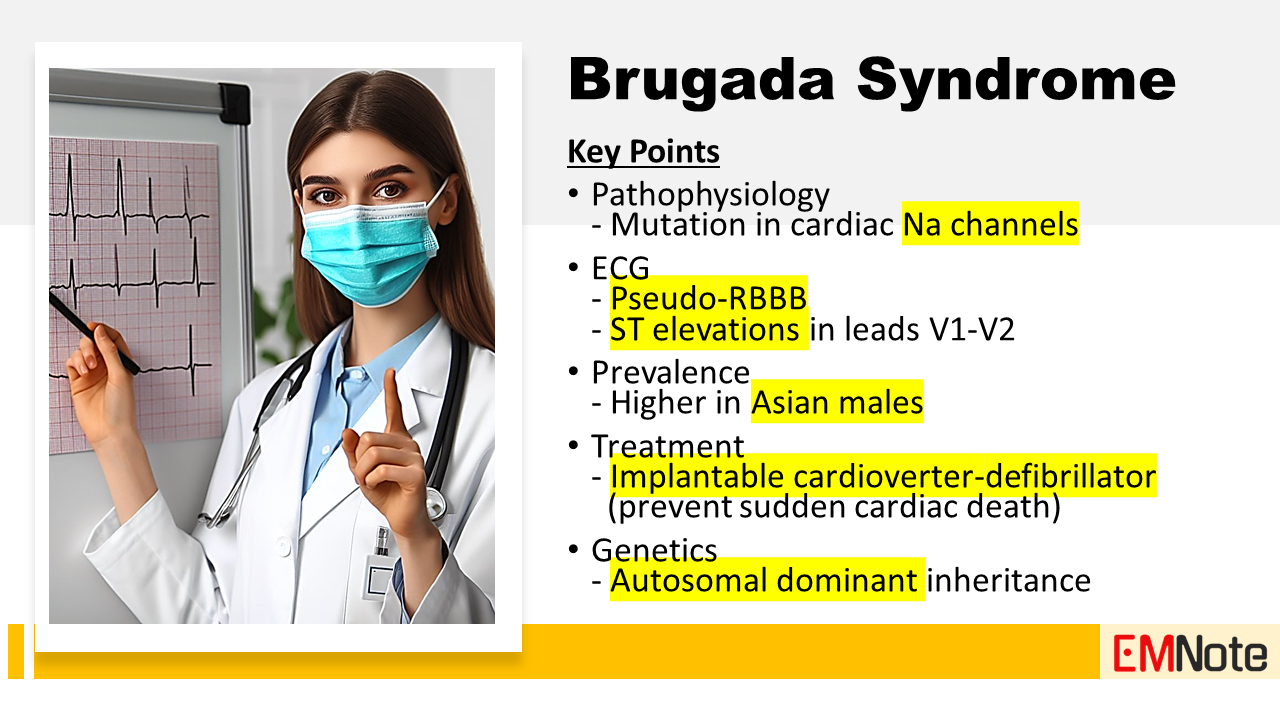
Brugada syndrome
Clinical manifestations
Diagnostic Tools of Brugada Syndrome
ECG Patterns of Brugada Syndrome
Diagnosis of Brugada Syndrome Brugada syndrome is diagnosed when type 1 Brugada ECG pattern is associated with one of the following clinical criteria:
Treatment of Brugada Syndrome
Conclusion
Airway Management Tips
Modified Valsalva Maneuver for PSVT
This modified Valsalva Maneuver is a simple yet effective technique used to treat stable PSVT. Phase 1: Increasing Intrathoracic Pressure.
Phase 2: Sudden Drop in Intrathoracic Pressure.
Phase 3: Laying Flat and Raising Legs to 45 Degrees.
In conclusion, by manipulating the nervous system and leveraging physiology, this maneuver is a safe, simple, and cost-free treatment to treat PSVT. Morel-Lavallee Lesion
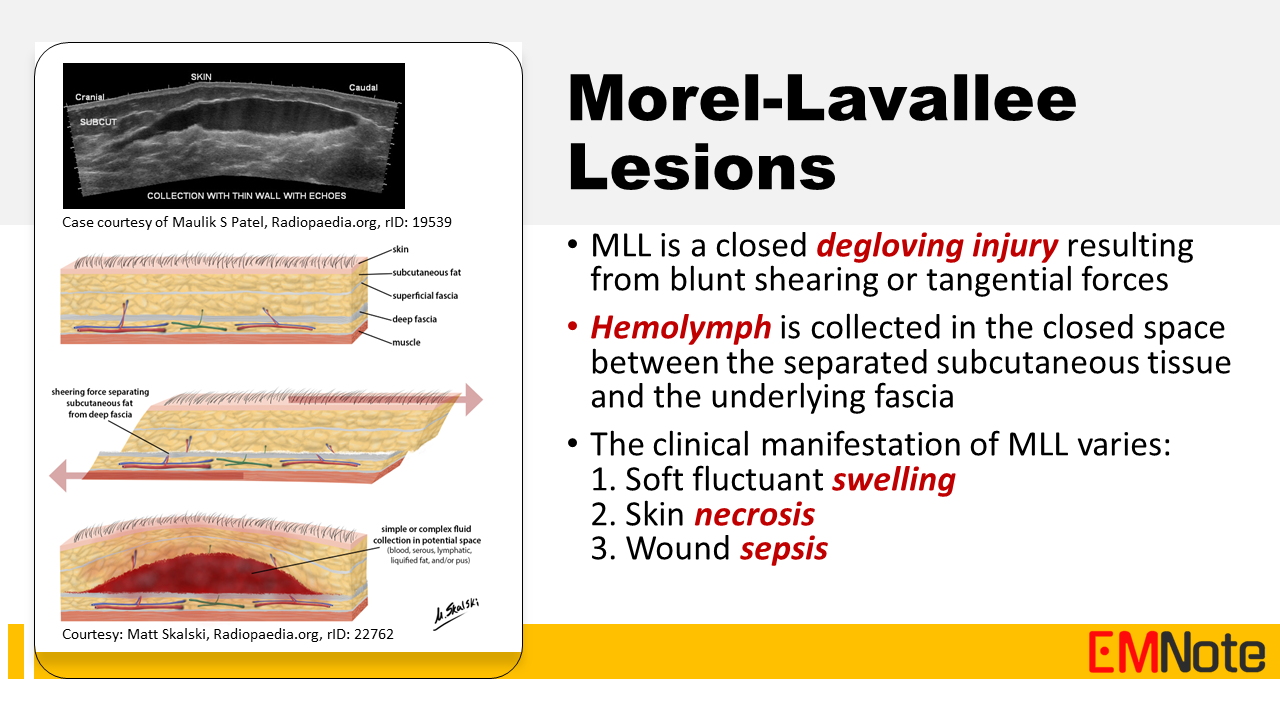
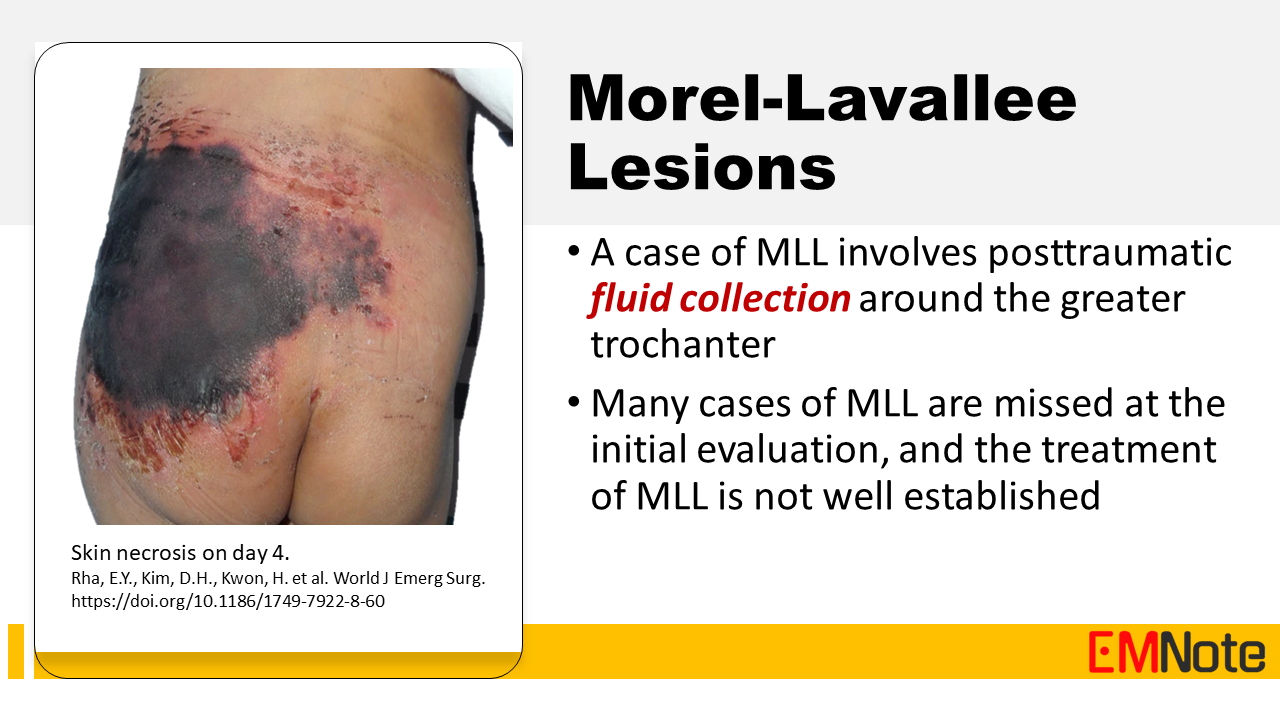
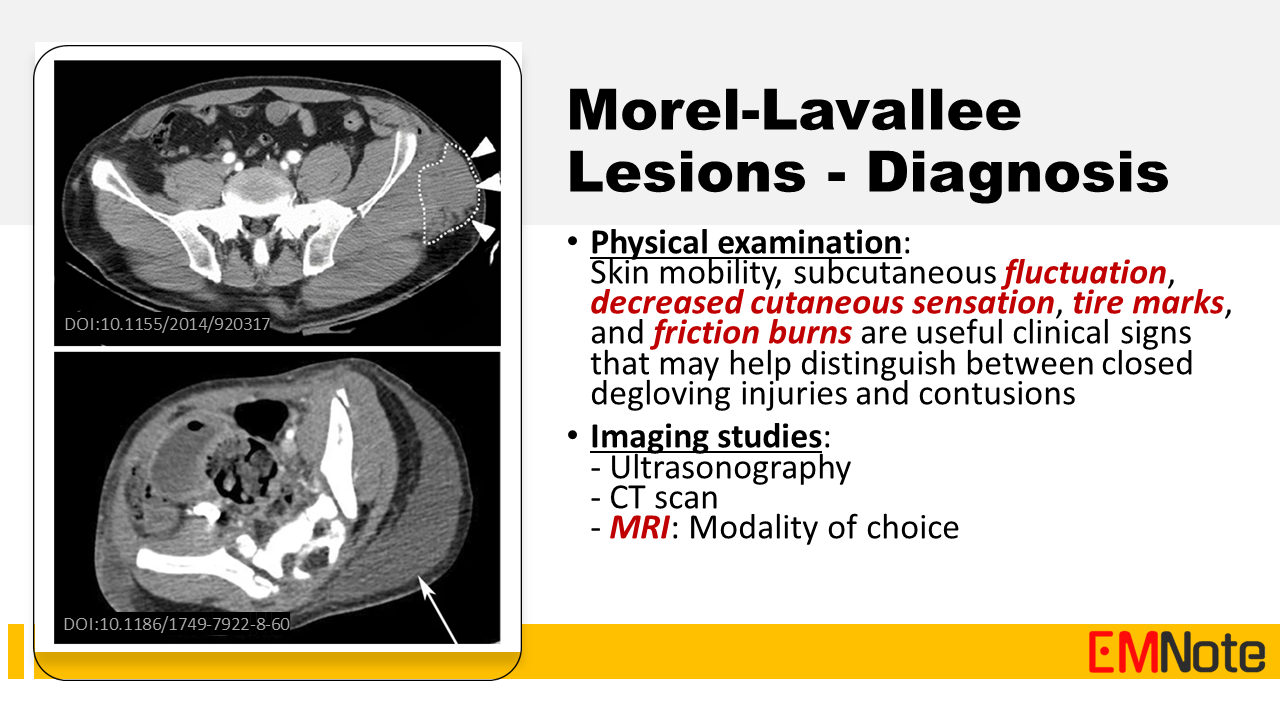
Background Morel-Lavallee lesion (MLL) is a closed degloving injury resulting from blunt shearing or tangential forces. In this condition, hemolymph is collected in the closed space between the separated subcutaneous tissue and the underlying fascia. MLL is associated with a potential risk of skin necrosis and soft tissue infection. Its clinical manifestation varies from soft fluctuant swelling to skin necrosis or wound sepsis. Physical examination Physical examination findings that may help distinguish between closed degloving injuries and contusions include: skin mobility, subcutaneous fluctuation, decreased cutaneous sensation, tire marks, and friction burns. Imaging studies for MLL include: Ultrasonography, CT scan, and MRI. MRI is the imaging technique of choice due to its superior soft tissue resolution and ability to identify the presence or absence of a capsule surrounding the fluid collection, which guides treatment decisions. Management Management of Morel-Lavallee lesions depends on several factors, including the size, location, and presence of complications. Nonoperative treatment with compression dressings, observation, and pain management is often sufficient for smaller lesions. However, larger or symptomatic lesions may require percutaneous aspiration or open surgical debridement to remove the fluid collection and prevent complications. Take Home Message Given their potential to mimic other conditions and contribute to surgical site infections, Morel-Lavallee lesions should be considered in the differential diagnosis for trauma patients presenting with soft tissue swelling, particularly in the prepatellar or hip regions. Early diagnosis and prompt initiation of appropriate management, including timely referral for definitive imaging and intervention, are crucial to prevent long-term complications and optimize patient outcomes. |

Author
|
Proudly powered by Weebly